Hashimoto’s disease, or autoimmune thyroiditis is the OG autoimmune disease. First described in 1912, Hashimoto’s was the first time we recognized that our immune system could turn on us and destroy our healthy tissue rather than the viruses and bacteria it is designed to destroy.
To this day, Hashimoto’s is also the most common autoimmune disease, and it impacts women far more often than men.
In this article, we’re going to be talking about some of the issues that women uniquely face with Hashimoto’s, and what we can do about it.
*If you want a quick primer on what is happening in Hashimoto’s, check out Understanding Hashimoto’s, and then come back. I’ll be here waiting.
Autoimmune Disease and Women
For most autoimmune diseases, not just Hashimoto’s, women far outnumber men. Why is that? It’s our hormones. Men and women’s physiology differ in many ways, but our hormone levels are one of the most significant differences.
Estrogen, that most female of the hormones, is known to be immune stimulating. Seems like a good thing – estrogen helps our immune system to produce more antibodies and inflammatory compounds essential for healing. But this is not a good thing when your immune system has lost the ability to recognize what is your healthy tissue and what is a virus, bacteria, or parasite. A dysregulated immune system, one that is capable of attacking our own healthy tissue, when stimulated by estrogen can be a powerful, destructive force. And one we need to regain control over.
Hashimoto’s and Hormones
The hormones in our bodies are engaging in a never-ending dance. No hormone acts in isolation, they each dance with each other – enhancing the effects of one hormone, suppressing the actions of another. It’s complex AF. And the belle of the ball is thyroid hormone.
Thyroid hormone influences, and is influenced by, just about every other hormone in our body – from stress-based cortisol, to sleepy melatonin, to period regulating progesterone and estrogen. These hormone relationships play out in various ways for women with Hashimoto’s.
Hashimoto’s and Periods
Hashimoto’s and other forms of hypothyroidism can mess up your periods. Two period irregularities are associated with hypothyroidism – irregular periods and heavy periods.
Irregular periods happen when your body doesn’t produce enough thyroid hormones. Making hormones and thickening the lining of the uterus in preparation for a baby are pretty energy-intensive projects for your body to undertake. When your thyroid hormones are low your body has to make decisions on what to spend its precious energy on – and baby making is not going to be one of them. So women can experience irregular cycles, or miss periods all together.
Heavy periods are another common consequence of Hashimoto’s and hypothyroidism. When we don’t produce enough thyroid hormones, we produce less progesterone, the hormone that lessens the amount of blood we lose during our period. We also produce less SHBG, a protein that binds to estrogen, leaving us exposed to more estrogen, which further thickens the lining of the uterus. As if that wasn’t enough, without adequate thyroid hormones, we may also make less coagulation factors necessary to prevent heavy periods. It’s a damn triple threat.
Hashimoto’s and The Pill
We’ve touched on the impact estrogen has on autoimmune disease; like putting gasoline on a fire, estrogen revs up our immune system with potentially disastrous consequences. And The Pill is one of the most potent sources of estrogen we could ever consider putting into our bodies.
Not only does the estrogen in The Pill impact our immune system, but estrogens also increase the production of a compound in our body called Thyroid Binding Globulin (TBG). This carrier molecule binds to our thyroid hormones, making them unavailable for us to use. This can lead us to feel the symptoms of hypothyroidism – weight gain, depression, fatigue – even when our thyroid hormone levels look normal on blood work.
For these reasons, I suggest women with Hashimoto’s consider alternate forms of contraception – condoms, fertility awareness method, or an IUD, and stay away from The Pill if possible.
Hashimoto’s and Pregnancy
In pregnancy we need thyroid hormones more than ever before. We’re making a human after all, and that is energy-intense work. So our T4 and T3 levels need to go up. For women with Hashimoto’s this can be a struggle, as much of the thyroid tissue may have been damaged or destroyed by autoimmune antibodies.
Women with Hashimoto’s may struggle to get pregnant or have an increased risk of miscarriage. TSH levels above 2.5 are associated with an increased risk of miscarriage, as are high TPO levels (one of the two autoimmune antibodies associated with Hashimoto’s.)
For women with Hashimoto’s who are considering pregnancy, I recommend speaking to your Naturopathic Doctor prior to trying to conceive. Spending a few months supporting your thyroid and balancing your immune system can go a long way towards helping you achieve your dreams of a healthy, happy pregnancy.
Hashimoto’s and Perimenopause
It is no surprise to me that the majority of diagnoses of Hashimoto’s occur for women between the ages of 30 and 50. This is a time of significant hormonal fluctuation, with progesterone levels declining and estrogen levels dominating. This leads to increased action of estrogen – or the dreaded estrogen dominance.
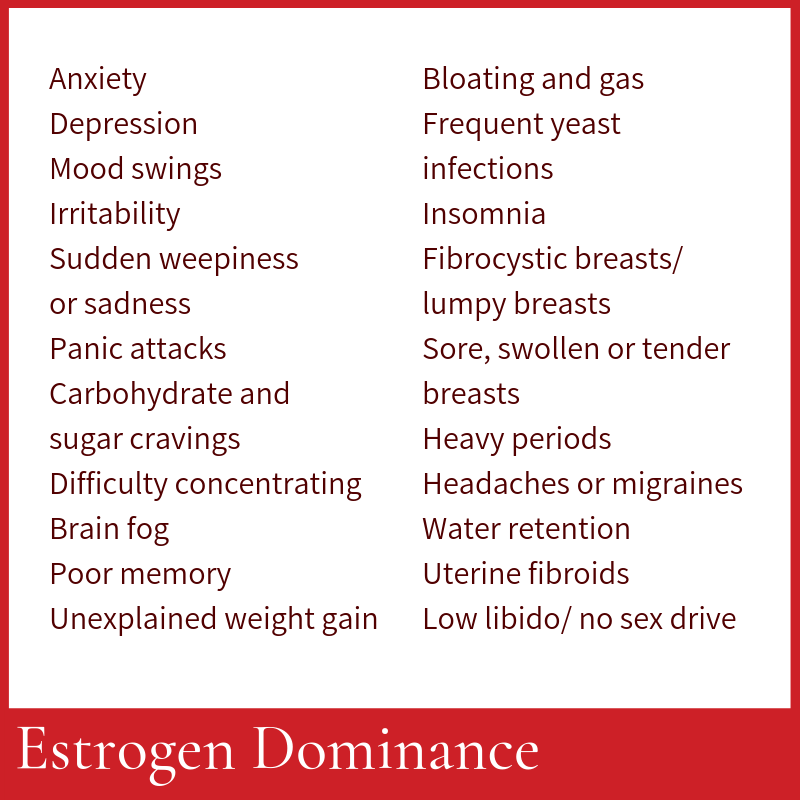
When progesterone levels decline, which begins around 25 for most women, we produce less thyroid hormones, especially T4. Combined with the immune stimulating effects of estrogen, this leaves women susceptible to the symptoms of hypothyroidism, and the tissue destruction of Hashimoto’s. And because of the significant overlap between symptoms of estrogen dominance and hypothyroidism, many women are never adequately diagnosed or supported for either of these hormone imbalances.
Hashimoto’s and Menopause
You would hope that the drop in estrogen levels at menopause would mean an improvement for women with Hashimoto’s. Alas, it’s more complicated than that. As our ovaries stop maturing eggs, the entire balance of hormones in our body is thrown into chaos. It becomes more difficult for us to produce thyroid hormones. It takes longer for us to convert T4 into active T3. And our ability to regulate inflammation created by our immune system also declines, which can worsen Hashimoto’s symptoms.
Empowering Women: Hormones and Hashimoto’s
It’s all well and good to understand how women are uniquely impacted by Hashimoto’s. But what is a woman to do? How can we support ourselves through the different stages of our hormonal journey?
1. Get comprehensive hormone testing.
Understanding the overall balance of our hormones is imperative to balancing this intricate and complex system. Blood tests and urine tests (like the DUTCH Test) can be incredibly valuable in understanding how to support your symptoms, your immune system, and your thyroid.
2. Know your antibody status.
One of my pet peeves is how few women know their antibody status in hypothyroidism. With most cases of hypothyroidism being autoimmune, knowing what antibodies you are producing is imperative to putting together a comprehensive plan. And these tests are just a quick blood draw away.
3. Skip The Pill
The high estrogen in oral contraceptives is a recipe for disaster for women with Hashimoto’s. Unless absolutely necessary, consider other options.
4. Avoid Nutritional Deficiencies
Deficiencies in many nutrients can cause, or worsen, Hashimoto’s. Discuss with your Naturopathic Doctor if you are getting enough selenium, iodine, iron, zinc, vitamin A, vitamin B12, vitamin E, folate, and tyrosine.
5. Work with an Expert
You are not a doctor (or maybe you are!) and you shouldn’t have to act like one. Navigating hormone imbalances and autoimmune diseases is complex, and working with an expert can help you achieve your goals faster, easier, and safer. You are a worthwhile investment. Get the help you need.
Selected references
- Poppe K, Velkeniers B, Glinoer D. Thyroid disease and female reproduction. Clin Endocrinol (Oxf). 2007 Mar;66(3):309–21.
- Brownstein D. Overcoming Thyroid Disorders. West Bloomfield, MI: Medical Alternatives Press; 2002.
- Mincer DL, Jialal I. Hashimoto’s Thyroiditis. StatPearls [internet]. https://www.ncbi.nlm.nih.gov/books/NBK459262/ Accessed January 13, 2021
- Schindler AE. Thyroid function and postmenopause. Gynecol Endocrinol. 2003 Feb;17(1):79-85. https://pubmed.ncbi.nlm.nih.gov/12724022/
- White HD, et al. CD3+ CD8+ CTL activity within the human female reproductive tract: influence of stage of the menstrual cycle and menopause, 1997
- Gameiro CM, Romao F, Castelo-Branco C. Menopause and aging: changes in the immune system—a review. Maturitas. 2010 Dec;67(4):316-20.
- Sammaritano LR. Menopause in patients with autoimmune diseases. Autoimmun Rev. 2012 May;11(6-7):A430-6.
Disclaimer
The advice provided in this article is for informational purposes only. It is meant to augment and not replace consultation with a licensed health care provider. Consultation with a Naturopathic Doctor or other primary care provider is recommended for anyone suffering from a health problem.