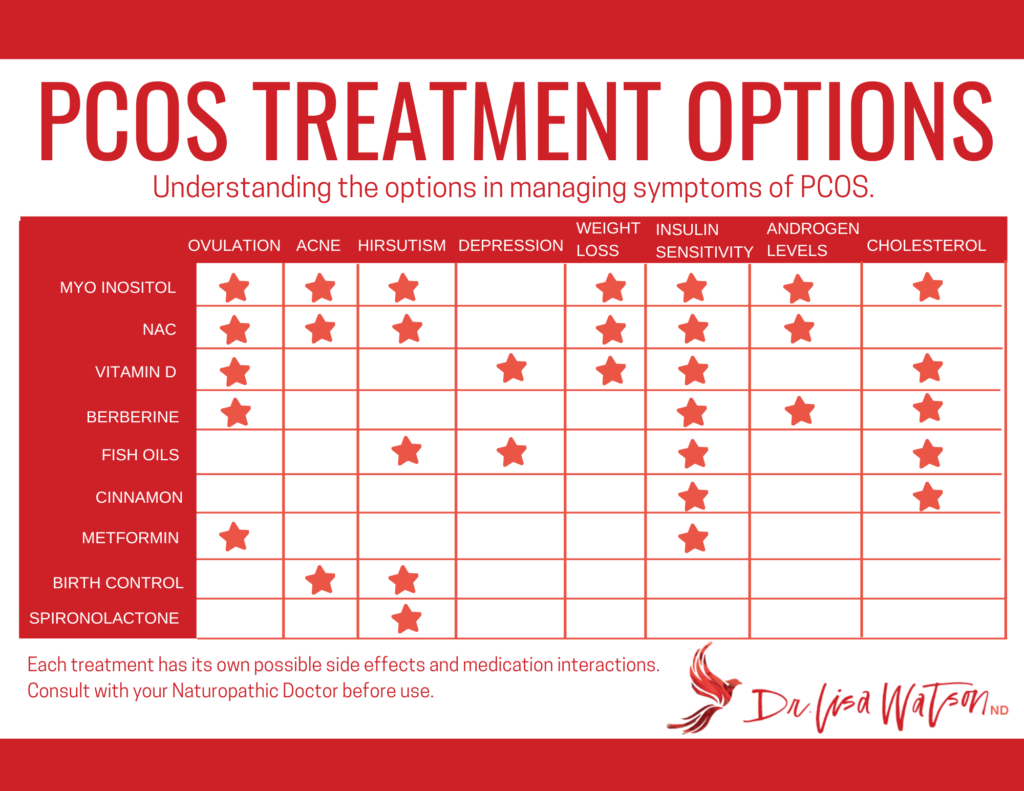
Every year more and more research is being done to help us understand the underlying causes, and potential treatments for PCOS. It is an exciting area of research, and we are recognizing that there are natural treatment options that perform as well, or better, than the current medications currently being prescribed to women with Polycystic Ovarian Syndrome. This article will help you to understand the most impactful treatments that are currently available, both natural and prescription, so that you can make the best choices for your own health.
Myo-Inositol
A unique molecule created in our bodies, inositol is a secondary insulin messenger, it impacts how our body uses insulin to regulate blood sugar. While most of us have heard of myo-inositol and d-chiro inositol, there are actually nine different forms of inositol in our bodies.
We know that women with PCOS tend to have altered inositol levels, especially lower myo-inositol in their bodies, and in particular in their follicular fluid. This impacts the ways that their bodies, and their ovaries, respond to insulin. This is likely something we inherit in our genetics, and is not something we caused by our diet or lifestyle choices.
A NOTE ON D-CHIRO INOSITOL
Our bodies convert myo-inositol into d-chiro inositol through a fancy little enzyme called eperimase. In women with PCOS levels of this enzyme can be increased, resulting in increased production of d-chiro inositol, at the expense of myo-inositol. The presence of increased d-chiro inositol can inhibit our aromatase enzyme and result in increased testosterone levels.
This is important because some people on the internet are advocating for formulas that include d-chiro inositol (so-called 40:1 ratios.) This is never recommended for PCOS as adding additional d-chiro inositol can potentially reduce egg quality, increase testosterone levels, and make it more challenging to achieve hormone balance in PCOS.
The research on myo-inositol in PCOS has given us a great understanding of why it is so beneficial for women. Some of the most profound benefits include:
- Improves insulin sensitivity, reduces fasting insulin
- Improves ovarian response to FSH
- Increases aromatase activity, increasing estrogen and decreasing testosterone
- Increases SHBG levels, further decreasing free testosterone
- Improves ovulation rates and menstrual regularity
- Improves egg quality (and pregnancy rates)
- Reduces rates of gestational diabetes in PCOS pregnancies
- Improves cholesterol levels, including triglycerides
While we do eat myo-inositol in our diets, even the most diligent of us consume only around 500-700mg per day. In clinical studies the typical effective dose is 2000-4000mg (or 2-4g) with women who are overweight potentially needing a bit more.
Myo-inositol does not work instantly, the best benefits are seen over 6 months, but research suggests that most women with PCOS will ovulate within the first 24-40 days on this supplement.
Myo-inositol should be taken away from meals, typically dosed morning and night. The most common side effect is bloating which can be minimized by slowly increasing the dosage over time, or taking it with an alpha lactoalbumin supplement (usually in the form of whey protein powder.) Folic acid is added to most treatment plans with myo-inositol as it can further support egg development.
Interestingly, when compared to one of the most common medications for PCOS, metformin, the results achieved with myo-inositol are very similar. They both improve blood sugar, insulin levels, ovulation and period regularity, and hormone levels. Myo-inositol may in fact be better than metformin at reducing elevated androgens and the symptoms associated with that hormone balance (acne, hirsutism, and hair loss.)
You will need to stay on the myo-inositol as long as you want to derive the benefits from it. Remember, PCOS is a genetic condition, and your body needs the myo-inositol for it to function optimally. If you can’t make it, you need to take it.
If you become pregnant while taking myo-inositol, do not discontinue it. Myo-inositol during pregnancy can reduce the incidence and severity of gestational diabetes and reduce the risk of miscarriage, which is significantly elevated in women with PCOS.
N-Acetyl Cysteine
N-acetyl cysteine (NAC) is a precursor for the conditionally essential amino acid cysteine. Used for its powerful antioxidant and anti-inflammatory effects, NAC is one of our cornerstone treatments for PCOS.
NAC has unique benefits for PCOS not found with other treatments, most notable improvements in endometrial lining thickness. Other benefits of NAC include:
- Improved insulin response
- Lowered androgens and improved symptoms of androgen balance
- Improved ovulation and menstrual regularity
- Improved fertility outcomes – better egg quality, reduced miscarriage rates, fewer drugs needed in fertility treatments, thicker endometrial lining, higher pregnancy and live birth rates
NAC has also been compared to metformin and found that it has similar pregnancy rates, similar reductions in total testosterone, and patients taking NAC had a greater reduction in body weight. NAC wasn’t as successful at lowering fasting insulin as metformin, but it still does benefit blood sugar balance and insulin sensitivity.
The dosage of NAC is usually 500mg given three times per day with meals. It should be taken for a minimum of three months to see benefit, with most benefit seen after six months. For women who are overweight, the dose may go up to 1000mg three times per day.
For women undergoing fertility treatment, improvements have been seen with NAC in as few as four days of supplementation. However, for most women, three months of supplementation is recommended before undergoing as assisted fertility cycle.
Unlike myo-inositol which is continued throughout pregnancy, NAC is used up until ovulation or oocyte retrieval in a fertility cycle, and then stopped. It can be resumed in the next month if pregnancy is not achieved.
Omega 3 Fatty Acids
Omega 3 fatty acids are essential fatty acids, meaning that they are essential for our bodies to function. As we don’t easily make omega 3s ourselves, we need to consume them in food, or take them as supplements.
For PCOS omega 3 fatty acids are most useful for improving mood – especially depression – associated with PCOS. Omega 3s have also been found in studies to improve fasting insulin, total testosterone, measures of inflammation, and the appearance of abnormal hair growth (hirsutism.)
With additional benefits in balancing cholesterol levels, and reducing fatty liver disease, omega 3 fatty acids are often incorporated into a holistic treatment plan for PCOS, but are rarely used on their own.
The most abundant source of omega 3 fatty acids in the diet is cold water fish – trout, mackerel, herring, salmon, and sardines. Some eggs are good sources, and plant based sources include walnuts, flax, chia, hemp seeds, and the oils made from these nuts and seeds. Most research studies use supplemental omega 3s with dosages ranging from 2000-3500mg per day.
Vitamin D
Vitamin D is one of the most important nutrients for hormonal conditions because it acts as a pro-hormone in our bodies, influencing the way that our hormones act. It also regulates genes that are crucial for blood sugar metabolism and fat metabolism (i.e. weight loss.) It is also one of the most common nutrient deficiencies, due to low sunlight exposure during the winter months and sunscreen usage in the summer months.
For women with PCOS, vitamin D can improve blood sugar stability and reduce insulin resistance, while also supporting healthy follicle development and cycle regularity. Vitamin D, through its actions on serotonin, has also been found to improve mood, and as depression and anxiety are more common in women with PCOS, this benefit is not to be ignored. For women considering pregnancy, improving vitamin D status was one of the most significant ways to reduce miscarriage rates and improve live birth rates (with a four-fold increase in birth rates for women with sufficient vitamin D in one study.)
It has been estimated in studies that up to 75% of women with PCOS are deficient in vitamin D. Deficiency is more common in women who are overweight as well. And while blood testing for vitamin D is not commonly done, it is recommended for all women with PCOS. Be mindful, however, that the “normal” lab range is not considered adequate for PCOS. In women with PCOS we want a minimum of 110nmol/L of vitamin D for positive benefits.
For most women a higher dosage is needed to achieve these blood levels of vitamin D. Dosing of 25 000
to 40 000IU are common in studies. Your dosage will be determined based on blood work, and your
body weight.
Berberine
One of the best researched botanical medicines for PCOS, berberine has a lot of potential benefits. Research over the past 20 years has shown that berberine can:
- Reduce total testosterone and increase SHBG
- Improve insulin sensitivity
- Decreased total cholesterol and improved HDL (“good” cholesterol)
- Improve ovulation rates
- Improvements in non-alcoholic fatty liver disease
Studies on berberine have found that it is comparable to metformin in improving ovulation rates, and may be more effective than metformin in reducing elevated testosterone and androgens. Some studies have even shown higher live birth rates in women with PCOS who were trying to conceive, compared to placebo and to women taking metformin.
Berberine is most effective when combined with other treatments, including NAC, myo-inositol, and Clomid. Studies have also shown improvements when combining berberine with lifestyle and dietary counseling.
For women who are trying to get pregnant, berberine should be stopped once you are pregnant, or after a transfer if you are doing IVF.
Cinnamon
The research on cinnamon for PCOS is somewhat lacking, however, with the known benefits on blood sugar stability from diabetes research, some information on using Cinnamon for PCOS is starting to emerge.
Cinnamon can help in balancing blood sugar and improving cholesterol for women with PCOS. However, there isn’t much evidence that cinnamon helps restore ovulation and cycle regularity for women with PCOS. It’s a nice part of your diet, but maybe isn’t impactful enough to use as a supplement just yet.
Metformin
A treatment for diabetes, metformin is used to balance blood sugar and reduce insulin resistance in women with PCOS. Most often used in women who are overweight, metformin can also be given at lower doses for women with lean PCOS, or teens with PCOS.
Metformin is often used in pregnancy for women with PCOS as it can reduce early pregnancy loss. It is known that using metformin reduces the diagnosis of gestational diabetes in women with PCOS, but it doesn’t seem to change meaningful outcomes – including rates of late miscarriage, preterm delivery, or birth weight.
In general, I don’t recommend metformin routinely for PCOS as there are other options, such as myo-inositol, and NAC, that perform at least as well, if not better than metformin, with fewer side effects and potentially more benefits.
Spironolactone
An aldosterone receptor antagonist, spironolactone is mostly used in the treatment of edema, high blood pressure, heart, and kidney disease. In PCOS it is used exclusively to reduce the appearance of hirsutism (abnormal hair growth patterns.)
It does not have benefits for ovulation, cholesterol, or insulin sensitivity. The most common side effect associated with spironolactone in women is mid-cycle bleeding, which can be confusing for women with PCOS who already have irregular cycles and may misinterpret this side effect.
Oral Contraceptives (“The Pill”)
While the pill is one of the most common treatment recommendations for PCOS, more and more women are opting for alternative treatments due to side effects and risks associated with the pill. While many women use the pill with no concerns, there are some facts about the pill that women with PCOS should consider:
- Birth control pills increase the risk of blood clots, and women with PCOS already have a 1.5 times higher baseline risk of clots (and a 3.7 times increased risk on the pill)
- The pill can increase cholesterol levels, a concern many women with PCOS already have
- Increased risk of depression associated with using the pill, again, a condition that PCOS also has an associated increased risk
- The progesterone only pill is associated with increased weight gain
- Increased risk of abnormal PAP tests with oral contraceptive use
- The “period” experienced on the pill is not a period, but a withdrawal bleed. It does not “normalize” cycles as many women are told.
The benefit of the pill is that it can protect women from one of the more harmful consequences of PCOS – endometrial cancer. When a woman with PCOS does not have a regular period, her uterine lining (endometrium) can be exposed to estrogen for prolonged periods of time, leading to an increased risk of precancerous changes. The birth control pill contains progestins, medications that are similar to progesterone, that protect the endometrium from the impacts of unopposed estrogen.
If you are considering the pill, be sure to get the preliminary testing done prior to best understand your risk factors associated with the pill. Your BMI, waist circumference, blood pressure, hirsutism score, fasting blood sugar, fasting cholesterol, and liver function tests should all be done before a prescription is made.
Disclaimer
The advice provided in this article is for informational purposes only. It is meant to augment and not replace consultation with a licensed health care provider. Consultation with a Naturopathic Doctor or other primary care provider is recommended for anyone suffering from a health problem.